Mysterious Vision Loss in Children linked to Covid-19?
A new medical mystery is emerging in pediatric care, Hyperacute Outer Retinal Dysfunction (HORD). It's a devastating condition that can rob children of their vision virtually overnight.
With every article and podcast episode, we provide comprehensive study materials: References, Executive Summary, Briefing Document, Quiz, Essay Questions, Glossary, Timeline, Cast, FAQ, Table of Contents, Index, Polls, 3k Image, and Fact Check.
A new medical mystery is emerging in pediatric care, and it's sending shockwaves through the medical community. Hyperacute Outer Retinal Dysfunction (HORDE) isn't just another complicated medical term – it's a devastating condition that can rob children of their vision virtually overnight.
The story begins with a six-year-old girl in China. One day, she's perfectly healthy. The next, following a simple fever, she can barely see. This isn't an isolated incident. Research published in JAMA Ophthalmology has documented eight children with similar experiences – sixteen eyes suddenly compromised, all following a fever.
What makes HORDE particularly troubling is its stealth and speed. Unlike other vision conditions that develop gradually, HORDE strikes with devastating swiftness. It affects both eyes simultaneously and targets specific parts of the retina – the ellipsoid zone and external limiting membrane. These aren't just random anatomical terms; they're crucial components of how our eyes process light and allow us to see.
But here's where things get even more concerning: COVID-19 might be involved.
Recent analysis suggests at least five possible connections between COVID-19 and HORDE. Two stand out as particularly compelling: First, COVID-19's notorious ability to trigger an overwhelming immune response could lead to friendly fire against the retina. Second, the virus's documented impact on blood vessels could disrupt crucial blood flow to the eye.
Think about that for a moment. We're not just talking about COVID's immediate effects anymore. We're looking at potential long-term consequences that could fundamentally alter children's lives.
The good news? Most children in the study showed significant improvement in their central vision within a year. The bad news? Their electroretinography (ERG) results – essentially their retinas' electrical activity – remained abnormal. Something was still wrong at a fundamental level, even after apparent recovery.
This raises uncomfortable questions about long-term impacts. If COVID-19 is indeed a trigger for HORDE, how many children might be at risk? Are we prepared to identify and treat these cases quickly enough?
Current treatments focus on suppressing the immune system through corticosteroids and other medications. But these are essentially educated guesses – we're still working to understand what actually causes HORDE.
There's a glimmer of hope in the discovery of specific antibodies (anti-PKC gamma and anti-RE) in some cases. These could serve as crucial biomarkers, potentially allowing earlier diagnosis and more targeted treatments. But we're not there yet.
The implications for public health are staggering. If even a small percentage of children who contract COVID-19 develop HORDE, we're looking at potentially thousands of cases worldwide. This isn't just a medical issue – it's a public health crisis waiting to happen.
What can we do? First, awareness is crucial. Parents and healthcare providers need to know about HORDE's existence and its warning signs. Early detection could make a significant difference in outcomes.
Second, we need comprehensive support systems. Vision rehabilitation, occupational therapy, and family counseling aren't optional extras – they're essential components of care for affected children and their families.
Finally, we need more research. The current studies, while groundbreaking, are just the beginning. We need larger, more diverse studies to understand HORDE's true scope and develop effective treatments.
This is where science meets reality. While researchers work to unlock HORDE's mysteries, real children and families are dealing with its impacts right now. They need support, understanding, and hope.
The message is clear: We can't wait for all the answers before taking action. We need to be proactive – in research, in medical care, and in support services. Because when it comes to children's vision, every moment counts.
The story of HORDE is still being written. But one thing is certain: The more we know, the better equipped we'll be to protect our children's vision and their futures.
Reference: Sudden vision loss in children: Study in China points to a novel retinal disorder by Justin Jackson , Medical Xpress
STUDY MATERIALS
1. Briefing Document
Executive Summary:
A recent study in China has characterized a novel retinal disorder in children, termed Hyperacute Outer Retinal Dysfunction (HORD), which is marked by sudden, severe bilateral vision loss following high fever illnesses. The condition involves disruptions to the photoreceptor layer of the retina. While most patients experience significant central vision recovery within a year, electroretinography (ERG) shows persistent extinguished rod and cone responses. The cause of HORD is unknown. A Perplexity AI assessment suggested potential links between HORD and COVID-19, via immune responses, vascular complications, neurological impacts, autoantibodies or post-viral syndrome. Further research is needed to determine the etiology, optimal treatment strategies, and long-term prognosis.
Main Themes & Key Ideas:
1. Hyperacute Outer Retinal Dysfunction (HORD): A Novel Retinal Disorder
Definition: HORD is characterized by sudden bilateral vision loss in children following a high fever.
Key Findings (Cheng et al., 2025):The study involved eight children (16 eyes) with no prior visual impairment who experienced sudden vision loss after febrile illnesses.
Initial visual acuity was severely reduced, often to the level of hand motions only.
"Comprehensive retinal imaging revealed characteristic ellipsoid zone (EZ) and external limiting membrane (ELM) disruptions."
"Electroretinography (ERG) findings demonstrated extinguished cone and rod responses, even in cases where vision improved."
Despite the initial severity, "At one year, 88% (7 of 8 patients) achieved visual acuity of 20/40 or better, with 50% (4 of 8) reaching 20/25 or better."
The “flying saucer sign” is associated with tapered foveal EZ with ELM
Diagnosis:Exclusion criteria include inherited retinal disease, uveitis, and white dot syndromes.
Differential diagnoses include multiple evanescent white dot syndrome (MEWDS), acute zonal occult outer retinopathy (AZOOR), and nonparaneoplastic autoimmune retinopathy (np-AIR), though HORD presents with more severe bilateral involvement than MEWDS or AZOOR, and a younger age of onset and hyperacute progression than np-AIR.
Potential Mechanism:Boyce and Han suggest that HORD may represent an inflammatory-mediated retinal disorder.
Early OCT findings, including vitritis, vascular sheathing, and intraretinal hyperreflective dots, point to acute inflammation.
Treatment:Patients received varying immunosuppressive treatments, including corticosteroids and intravenous immunoglobulin (IVIG).
The study notes that "a definitive therapeutic effect of treatment remained unclear."
2. Unknown Etiology & Need for Further Research
Systemic evaluations of the patients were "unremarkable," and "no infectious or autoimmune triggers were identified."
Two patients tested positive for specific antiretinal antibodies (antiPKC γ and antiRi), but the significance of this finding requires further investigation.
Further research is needed to determine the etiology, optimal treatment strategies, and long-term prognosis.
Identifying specific biomarkers, including potential novel antiretinal antibodies, may provide insight into disease mechanisms and therapeutic targets.
3. Potential Link to COVID-19 (Perplexity AI Assessment)
A Perplexity AI inquiry proposed several mechanisms by which sudden vision loss following high fever illnesses (specifically HORD) could be linked to COVID-19 infection:
Immune Response: "COVID-19 can trigger an exaggerated immune response, leading to inflammation. This hyper-inflammatory state may contribute to retinal damage..."
Vascular Complications: "COVID-19 is known to affect the vascular system, potentially causing vasculitis or thrombosis, which could compromise blood flow to the retina and result in vision loss."
Neurological Impacts: "The virus can affect the nervous system, leading to neurological symptoms. If the optic nerve or other visual pathways are impacted, this could result in sudden vision loss."
Autoantibodies: "Some patients with COVID-19 develop autoantibodies, which may cross-react with retinal proteins, potentially leading to autoimmune responses that could damage photoreceptors."
Post-Viral Syndrome: "Similar to other viral infections, COVID-19 may lead to post-viral syndromes, where persistent symptoms occur after the acute infection has resolved. This could include ocular symptoms and vision-related issues."
Implications:
The identification of HORD as a distinct retinal disorder is significant, especially given the potential for significant visual recovery.
Further research is crucial to determine the cause of HORD and to develop targeted treatments.
The potential link to COVID-19, as suggested by Perplexity AI, warrants further investigation, especially given the widespread nature of COVID-19 infections.
Clinicians should be aware of HORD and consider it in the differential diagnosis of children presenting with sudden vision loss following a febrile illness.
Next Steps:
Investigate the prevalence of HORD in different populations, particularly in regions with high COVID-19 infection rates.
Conduct further research to identify specific biomarkers and genetic factors associated with HORD.
Evaluate the efficacy of different treatment strategies for HORD, including corticosteroids, IVIG, and other immunosuppressive agents.
Explore the potential role of COVID-19 infection in the development of HORD through epidemiological and mechanistic studies.
2. Quiz & Answer Key
I. Review Topics
Hyperacute Outer Retinal Dysfunction (HORD): Definition, key characteristics, and diagnostic criteria.
Clinical Presentation of HORD: Sudden vision loss, age of onset, bilateral involvement.
Retinal Imaging Findings in HORD: Ellipsoid zone (EZ) and external limiting membrane (ELM) disruptions, OCT findings, fundus appearance.
Electroretinography (ERG) Results in HORD: Rod and cone responses.
Potential Etiology of HORD: Inflammatory mechanisms, autoimmune responses, viral association (including potential links to COVID-19).
Differential Diagnosis: Distinguishing HORD from other retinal disorders (MEWDS, AZOOR, np-AIR).
Treatment Strategies for HORD: Immunosuppressive therapies (corticosteroids, IVIG).
Prognosis of HORD: Visual recovery, long-term outcomes.
COVID-19 and Retinal Disorders: Potential mechanisms linking COVID-19 to retinal damage (immune response, vascular complications, neurological impacts, autoantibodies, post-viral syndrome).
Research Directions: Identifying biomarkers, optimal treatment strategies, understanding disease mechanisms.
II. Quiz
Answer the following questions in 2-3 sentences each.
What is the primary characteristic defining Hyperacute Outer Retinal Dysfunction (HORD)?
What are the typical changes observed in the ellipsoid zone (EZ) and external limiting membrane (ELM) in patients with HORD, as revealed by OCT imaging?
Describe the findings of electroretinography (ERG) in HORD cases, even after visual improvement.
What other conditions are used for differential diagnosis with HORD?
What are the primary immunosuppressive treatments used for HORD, and what is the certainty of their effectiveness?
According to the commentary by Boyce and Han, what potential mechanism might be driving retinal damage in HORD?
What are some of the proposed mechanisms by which COVID-19 infection could be linked to sudden vision loss in children?
What criteria were used to exclude the study participants and isolate this novel retinal disorder, HORD?
What antiretinal antibodies are associated with the HORD study?
Describe the "flying saucer sign" in relation to the EZ and ELM?
III. Quiz Answer Key
HORD is primarily characterized by sudden, bilateral vision loss in children, often following a febrile illness. It involves disruptions in the outer retina, particularly the photoreceptor layer.
OCT imaging in HORD typically reveals disruptions in the ellipsoid zone (EZ) and external limiting membrane (ELM) of the retina. These disruptions indicate damage to the photoreceptor cells.
Even after visual improvement in HORD, electroretinography (ERG) often shows extinguished rod and cone responses. This suggests persistent dysfunction at the photoreceptor level despite restored visual acuity.
Conditions considered in the differential diagnosis of HORD include multiple evanescent white dot syndrome (MEWDS), acute zonal occult outer retinopathy (AZOOR), and nonparaneoplastic autoimmune retinopathy (np-AIR). However, HORD's presentation with severe bilateral involvement and hyperacute onset helps distinguish it.
Corticosteroids and intravenous immunoglobulin (IVIG) are the primary immunosuppressive treatments used for HORD. The study indicates there is no certainty to their effectiveness.
Boyce and Han suggest that HORD may represent a novel inflammatory-mediated retinal disorder, potentially involving acute inflammation as a driver of retinal damage. They describe HORD as "A Retina on Fire."
COVID-19 could be linked to sudden vision loss through mechanisms like an exaggerated immune response leading to retinal inflammation, vascular complications affecting retinal blood flow, neurological impacts on the optic nerve, autoantibody development targeting retinal proteins, and post-viral syndromes with ocular symptoms.
Exclusion criteria included inherited retinal disease, uveitis, and white dot syndromes, to isolate this as a novel retinal disorder, HORD.
The antiretinal antibodies antiPKC γ and antiRi are associated with the HORD study.
The “flying saucer sign” refers to the tapered appearance of the foveal EZ with ELM disruption, resembling a flying saucer, observed in OCT imaging of HORD patients at the 12 month mark.
3. Essay Questions
Discuss the potential mechanisms underlying the development of Hyperacute Outer Retinal Dysfunction (HORD), considering both the study findings and the commentary by Boyce and Han.
Compare and contrast Hyperacute Outer Retinal Dysfunction (HORD) with other retinal disorders such as MEWDS, AZOOR, and np-AIR, highlighting the key differentiating features of HORD.
Evaluate the potential role of COVID-19 infection in the development of retinal disorders like HORD, exploring the proposed mechanisms and potential future research directions.
Analyze the limitations of the current study on HORD, focusing on sample size, lack of identified triggers, and the unclear therapeutic effect of treatments.
Based on the existing research, propose future research directions for HORD, including potential biomarkers, optimal treatment strategies, and methods for understanding disease mechanisms.
4. Glossary of Key Terms
Hyperacute Outer Retinal Dysfunction (HORD): A distinct retinal disorder characterized by sudden, bilateral vision loss in children following high fever illness, marked by photoreceptor disruption.
Best-Corrected Visual Acuity (BCVA): The sharpest vision a person can achieve with the help of corrective lenses (glasses or contacts).
Ellipsoid Zone (EZ): A layer of the photoreceptors in the retina, visible on OCT imaging, that is critical for visual function. Damage to the EZ is often associated with vision loss.
External Limiting Membrane (ELM): A boundary layer in the retina that separates the photoreceptor cells from other retinal cells. Its integrity is important for retinal structure and function.
Optical Coherence Tomography (OCT): An imaging technique that uses light waves to capture high-resolution cross-sectional images of the retina.
Electroretinography (ERG): A diagnostic test that measures the electrical activity of the retina in response to light stimulation. It helps assess the function of photoreceptor cells (rods and cones).
Multiple Evanescent White Dot Syndrome (MEWDS): An inflammatory condition affecting the retina, characterized by small, white dots in the outer retina and transient vision loss.
Acute Zonal Occult Outer Retinopathy (AZOOR): A rare retinal disorder characterized by sudden vision loss and visual field defects, often with minimal or no visible changes in the retina.
Nonparaneoplastic Autoimmune Retinopathy (np-AIR): A retinal disorder caused by autoantibodies that attack the retina, leading to progressive vision loss. It is not associated with cancer.
Immunosuppressive Treatment: Therapy that suppresses the immune system, often used to treat autoimmune and inflammatory disorders. Examples include corticosteroids and intravenous immunoglobulin (IVIG).
Photoreceptors: Specialized cells in the retina (rods and cones) that convert light into electrical signals that are sent to the brain for visual processing.
Vasculitis: Inflammation of blood vessels.
Thrombosis: The formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system.
Autoantibodies: Antibodies produced by the immune system that are directed against the body's own tissues or cells.
Nyctalopia: Night blindness; difficulty seeing in low light conditions.
Dyschromatopsia: Color blindness; impaired color vision.
Vitritis: Inflammation of the vitreous humor, the clear gel that fills the space between the lens and the retina of the eye.
Vascular Sheathing: The appearance of blood vessels that are surrounded by a whitish or opaque material.
Intraretinal Hyperreflective Dots: Small, bright spots within the retinal layers seen on OCT imaging, often indicative of inflammation or other pathological processes.
Antiretinal antibodies: Antibodies that target components of the retina.
5. Timeline of Main Events
Early 2025 (prior to study publication): Eight children in China are referred to pediatric retina services after experiencing sudden, severe vision loss. All patients experienced high fever illnesses roughly two weeks prior to presentation.
Initial Presentation: Patients present with hyperacute (sudden onset) bilateral vision loss. Mean visual acuity is below the ability to count fingers correctly. Retinal imaging shows disruptions in the ellipsoid zone (EZ) and external limiting membrane (ELM). Electroretinography (ERG) shows extinguished cone and rod responses. Systemic evaluations are unremarkable.
Week 3: Blurred EZ and ELM are observed via OCT imaging.
Week 4: Signs of macular recovery appear.
Within the First Year: Most patients (88%) achieve visual acuity of 20/40 or better; 50% reach 20/25 or better. Macular EZ and ELM appear intact in most eyes, though extrafoveal regions may remain affected.
1 Year Follow Up: Retinal imaging shows restored but disrupted EZ and ELM. ERG continues to show extinguished rod and cone responses, despite visual improvement.
Month 12: Tapered foveal EZ with ELM (flying saucer sign) observed via OCT imaging.
2024: Researchers conduct a multicenter study in China examining these cases. They characterize the condition as Hyperacute Outer Retinal Dysfunction (HORD). The study is published in JAMA Ophthalmology. A commentary article by Timothy Boyce and Ian Han is also published in JAMA Ophthalmology.
2024: The study findings are reported by Justin Jackson, Medical Xpress.
Present: Researchers are considering whether this is a novel inflammatory-mediated retinal disorder, and further research is needed to determine HORD's etiology, optimal treatment strategies, and long-term prognosis.
Cast of Characters
Justin Jackson: Author of the Medical Xpress article, "Sudden vision loss in children: Study in China points to a novel retinal disorder." He reported on the Chinese study that characterized HORD.
Yizhe Cheng: Lead researcher (or part of the research team) from the State Key Laboratory of Ophthalmology in China. Author of the JAMA Ophthalmology study, "Hyperacute Outer Retinal Dysfunction."
Timothy Boyce: Co-author of the commentary article, "Hyperacute Outer Retinal Dysfunction —A Retina on Fire," published in JAMA Ophthalmology. Affiliated with the University of Iowa.
Ian Han: Co-author of the commentary article, "Hyperacute Outer Retinal Dysfunction —A Retina on Fire," published in JAMA Ophthalmology. Affiliated with the University of Iowa.
Eight Children (Un-named): Patients who experienced the novel retinal disorder (HORD) and were the subjects of the study. They experienced sudden vision loss after a high fever illness.
6. FAQ
1. What is Hyperacute Outer Retinal Dysfunction (HORD), and what are its key characteristics?
HORD is a newly characterized retinal disorder affecting children, marked by sudden bilateral vision loss following a high fever illness. Key characteristics include: hyperacute (rapid onset) vision loss, disruption of photoreceptors (specifically the ellipsoid zone (EZ) and external limiting membrane (ELM)), and variability in the extent of visual recovery. Electroretinography (ERG) shows extinguished cone and rod responses even when vision improves.
2. What are the typical symptoms and clinical findings associated with HORD at initial presentation?
At presentation, patients typically exhibit severe, sudden-onset vision loss, often described as below the ability to count fingers. Common symptoms may include nyctalopia (night blindness), visual field constriction, and dyschromatopsia (color vision deficiency). Optical coherence tomography (OCT) imaging reveals diffuse loss of the EZ and ELM layers of the retina. Early fundus findings might be largely unremarkable before later changes appear.
3. What are the proposed causes or potential triggers for HORD, and what role might fever play?
While the exact etiology of HORD remains unknown, a high fever illness appears to be a consistent precursor. Research suggests an inflammatory-mediated mechanism may be involved, potentially described as a "retina on fire". Systemic evaluations of patients have been unremarkable for other infectious or autoimmune triggers, though some have tested positive for antiretinal antibodies. COVID-19 is one potential trigger for these mechanisms.
4. How does HORD compare to other retinal diseases like MEWDS, AZOOR, and autoimmune retinopathy?
HORD has some overlapping features with other retinal diseases, but also has distinct characteristics. Unlike multiple evanescent white dot syndrome (MEWDS) or acute zonal occult outer retinopathy (AZOOR), HORD presents with more severe bilateral involvement and only partial recovery. While some characteristics overlap with nonparaneoplastic autoimmune retinopathy (np-AIR), the pediatric age of onset and hyperacute progression distinguish HORD.
5. What treatments are currently used for HORD, and what is known about their effectiveness?
The main treatments used for HORD involve immunosuppression, including corticosteroids and intravenous immunoglobulin (IVIG). However, the study suggests that the definitive therapeutic effect of these treatments remains unclear. The treatment was administered to most patients in the study, but researchers could not definitively state the efficacy of these treatments.
6. What is the typical visual prognosis for children with HORD?
The visual prognosis for children with HORD appears to be relatively positive in many cases, with significant central vision recovery often occurring over one year. In the study, 88% of patients achieved visual acuity of 20/40 or better at one year, and 50% reached 20/25 or better. Macular EZ and ELM appeared intact in many eyes, though extrafoveal regions could still be affected. However, ERG often continues to show extinguished rod and cone responses despite visual improvement.
7. How might COVID-19 infection be related to conditions like HORD, and what are the potential mechanisms involved?
COVID-19 infection could potentially be linked to HORD-like conditions through several mechanisms. These include an exaggerated immune response leading to retinal inflammation, vascular complications (vasculitis or thrombosis compromising retinal blood flow), neurological impacts affecting the optic nerve, the development of autoantibodies that cross-react with retinal proteins, and post-viral syndromes that manifest as ocular and vision-related issues.
8. What further research is needed to better understand and manage HORD?
Further research is crucial to determine the exact etiology of HORD, develop optimal treatment strategies, and understand the long-term prognosis. Identifying specific biomarkers, including novel antiretinal antibodies, may provide insight into disease mechanisms and therapeutic targets. Understanding the triggers and potential causes are vital to preventing the disease.
7. Table of Contents with Timestamps
Introduction and Case Overview [0:00]
Overview of Heliox podcast's mission and introduction to HORDE as a sudden vision loss condition in children
Initial Case Study [1:45]
Discussion of the six-year-old girl in China and introduction to key symptoms
Clinical Findings [3:30]
Detailed examination of the JAMA study findings, including affected retinal areas and ERG results
The COVID-19 Connection [7:15]
Analysis of potential links between COVID-19 and HORDE, focusing on immune response and vascular damage
Treatment Approaches [12:45]
Current treatment methods, including immunosuppressive therapies and their effectiveness
Support Systems [16:30]
Discussion of vision rehabilitation, occupational therapy, and family support services
Research Questions [19:15]
Exploration of unanswered questions and areas requiring further study
Antibody Discovery [22:30]
Analysis of anti-retinal antibodies as potential biomarkers and treatment targets
Public Health Implications [27:45]
Broader impact on healthcare systems and need for increased awareness
Future Directions [31:00]
Discussion of necessary changes in research, healthcare access, and support systems
Closing Thoughts [34:15]
Final reflections on the importance of continued research and hope for affected families
8. Index with Timestamps
Antibodies
- anti-PKC gamma, 22:30, 23:15
- anti-retinal, 22:30, 23:45, 24:10
- biomarkers, 23:30, 24:00, 24:45
Blood vessels
- COVID-19 effects on, 8:45, 9:15
- damage to, 9:30, 10:15
- retinal flow, 9:45
COVID-19
- immune response, 8:15, 8:45
- long-term effects, 10:30, 11:15
- potential connection, 7:15, 8:00
Electroretinography (ERG)
- abnormal results, 4:45, 5:15
- definition, 5:30
- testing, 4:30
HORDE (Hyperacute Outer Retinal Dysfunction)
- characteristics, 2:45, 3:15
- diagnosis, 3:30, 4:00
- onset, 2:15, 2:45
Immune system
- autoimmune response, 8:15, 8:45
- overreaction, 8:30, 9:00
- suppression treatment, 13:15, 13:45
JAMA Ophthalmology study
- case studies, 2:00, 2:30
- findings, 3:30, 4:15
- patient outcomes, 4:45, 5:15
Retina
- damage patterns, 3:45, 4:15
- ellipsoid zone, 3:30
- external limiting membrane, 3:30
Support services
- counseling, 16:45, 17:15
- occupational therapy, 16:30, 17:00
- vision rehabilitation, 16:30, 17:30
Treatment
- corticosteroids, 13:15, 13:45
- immunosuppressive therapy, 13:00, 13:30
- outcomes, 14:15, 14:45
Vision loss
- central vision, 4:45, 5:15
- recovery patterns, 4:30, 5:00
- sudden onset, 2:15, 2:45
9. Poll
1. What concerns you most about HORD?
- Sudden onset in children
- Possible COVID-19 connection
- Long-term vision effects
2. Which research priority is most urgent?
- Finding exact cause
- Developing targeted treatments
- Early detection methods
3. How should we improve kids' eye care?
- More frequent screenings
- Better parent education
- Enhanced post-COVID monitoring
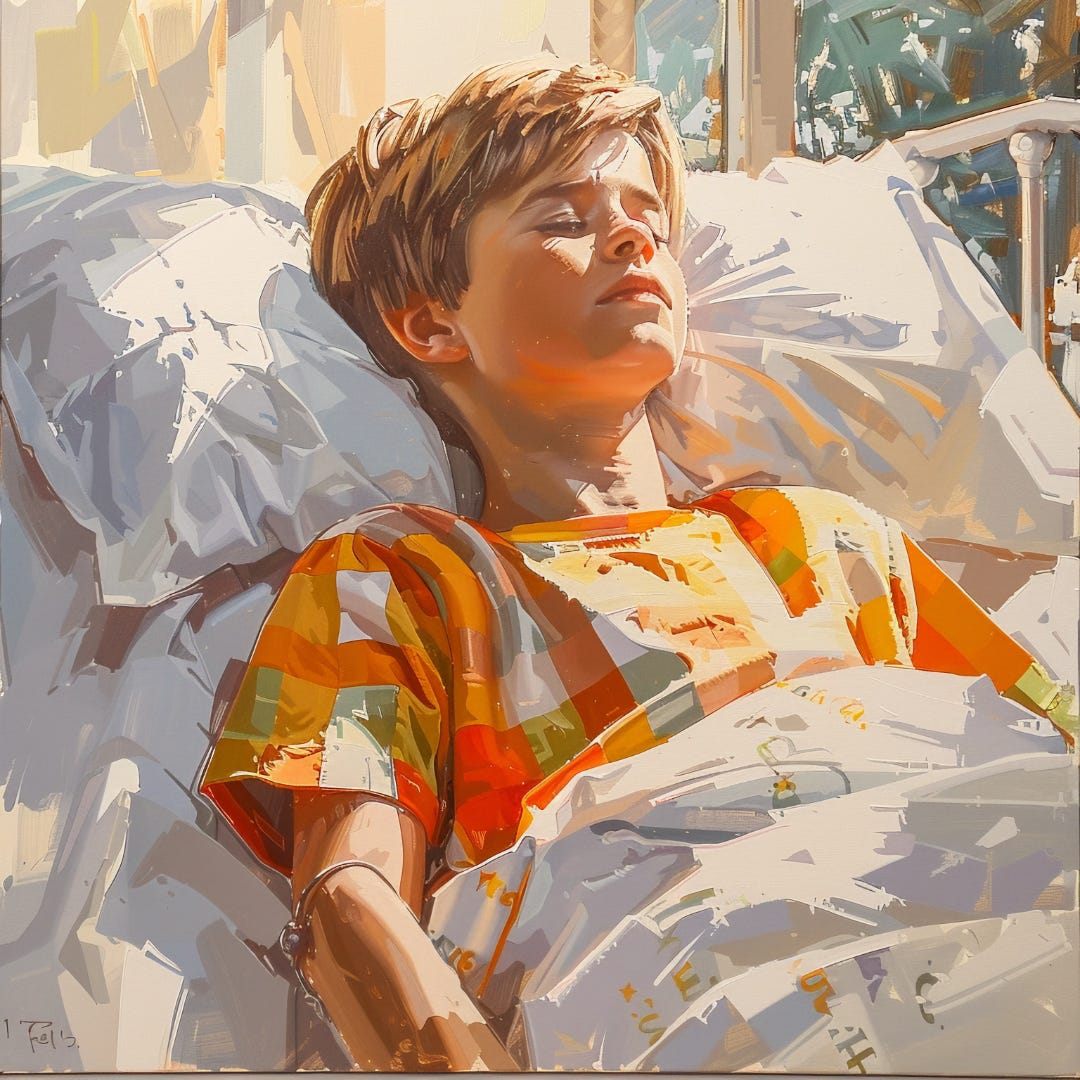
10. Image (3000 x 3000 pixels)
11. Post-Episode Fact Check
Overall, the content of the episode reflects the findings of the study and offers a thoughtful discussion on HORD, its implications, and the need for further investigation.